Urinary tract infection
A urinary tract infection (UTI), also known as acute cystitis or bladder infection, is an infection that affects part of the urinary tract.[1] When it affects the lower urinary tract it is known as a simple cystitis (a bladder infection) and when it affects the upper urinary tract it is known as pyelonephritis (a kidney infection). Symptoms from a lower urinary tract include painful urination and either frequent urination or urge to urinate (or both); while the symptoms of pyelonephritis include fever and flank pain in addition to the symptoms of a lower UTI. In some cases, a painful burning sensation in the urethra may be present even when not urinating. In the elderly and the very young, symptoms may be vague or non-specific. The main causal agent of both types is Escherichia coli, though other bacteria, viruses or fungi may rarely be the cause.
Urinary tract infections occur more commonly in women than men, with half of women having at least one infection at some point in their lives. Recurrences are common. Risk factors include female anatomy, sexual intercourse and family history. Pyelonephritis, if it occurs, usually follows a bladder infection but may also result from a blood-borne infection. Diagnosis in young healthy women can be based on symptoms alone. In those with vague symptoms, diagnosis can be difficult because bacteria may be present without there being an infection. In complicated cases or if treatment has failed, a urine culture may be useful. In those with frequent infections, low dose antibiotics may be taken as a preventative measure.
In uncomplicated cases, urinary tract infections are easily treated with a short course of antibiotics, although resistance to many of the antibiotics used to treat this condition is increasing. In complicated cases, a longer course or intravenous antibiotics may be needed, and if symptoms have not improved in two or three days, further diagnostic testing is needed. In women, urinary tract infections are the most common form of bacterial infection with 10% developing urinary tract infections yearly. In those who have bacteria or white blood cells in their urine but have no symptoms, antibiotics are generally not needed, although pregnant women are an exception to this recommendation.
Signs and symptoms
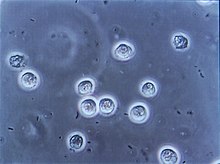
Urine may contain pus (a condition known as pyuria) as seen from a person with sepsis due to a urinary tract infection.
Lower urinary tract infection is also referred to as a bladder infection. The most common symptoms are burning with urination and having to urinate frequently (or an urge to urinate) in the absence of vaginal discharge and significant pain.[2] These symptoms may vary from mild to severe[3] and in healthy women last an average of six days.[4] Some pain above the pubic bone or in the lower back may be present. People experiencing an upper urinary tract infection, or pyelonephritis, may experience flank pain, fever, or nausea and vomiting in addition to the classic symptoms of a lower urinary tract infection.[3] Rarely the urine may appear bloody[5] or contain visible pus in the urine.[6]
Children
In young children, the only symptom of a urinary tract infection (UTI) may be a fever. Because of the lack of more obvious symptoms, when females under the age of two or uncircumcised males less than a year exhibit a fever, a culture of the urine is recommended by many medical associations. Infants may feed poorly, vomit, sleep more, or show signs of jaundice. In older children, new onset urinary incontinence (loss of bladder control) may occur.[7]
Elderly
 Urinary tract symptoms are frequently lacking in the elderly.[8] The presentations may be vague with incontinence, a change in mental status, or fatigue as the only symptoms,[3] while some present to a health care provider with sepsis, an infection of the blood, as the first symptoms.[5] Diagnosis can be complicated by the fact that many elderly people have preexisting incontinence or dementia.[8] It is reasonable to obtain a urine culture in those with signs of systemic infection that may be unable to report urinary symptoms, such as when advanced dementia is present.[9] Systemic signs of infection include a fever or increase in temperature of more than 1.1 °C (2.0 °F) from usual, chills, and an increase white blood cell count.[9]
Urinary tract symptoms are frequently lacking in the elderly.[8] The presentations may be vague with incontinence, a change in mental status, or fatigue as the only symptoms,[3] while some present to a health care provider with sepsis, an infection of the blood, as the first symptoms.[5] Diagnosis can be complicated by the fact that many elderly people have preexisting incontinence or dementia.[8] It is reasonable to obtain a urine culture in those with signs of systemic infection that may be unable to report urinary symptoms, such as when advanced dementia is present.[9] Systemic signs of infection include a fever or increase in temperature of more than 1.1 °C (2.0 °F) from usual, chills, and an increase white blood cell count.[9]
Cause
E. coli is the cause of 80–85% of community-acquired urinary tract infections, with Staphylococcus saprophyticus being the cause in 5–10%.[2] Rarely they may be due to viral or fungal infections.[10] Healthcare-associated urinary tract infections (mostly related to urinary catheterization) involve a much broader range of pathogens including: E. coli (27%), Klebsiella (11%), Pseudomonas (11%), the fungal pathogen Candida albicans (9%), and Enterococcus (7%) among others.[5][11][12] Urinary tract infections due to Staphylococcus aureus typically occur secondary to blood-borne infections.[3] Chlamydia trachomatis and Mycoplasma genitalium can infect the urethra but not the bladder.[13] These infections are usually classified as a urethritis rather than urinary tract infection.
Sex
In young sexually active women, sexual activity is the cause of 75–90% of bladder infections, with the risk of infection related to the frequency of sex.[2] The term "honeymoon cystitis" has been applied to this phenomenon of frequent UTIs during early marriage. In post-menopausal women, sexual activity does not affect the risk of developing a UTI. Spermicide use, independent of sexual frequency, increases the risk of UTIs.[2] Diaphragm use is also associated.[14] Condom use without spermicide or use of birth control pills does not increase the risk of uncomplicated urinary tract infection.[2][15]
Women are more prone to UTIs than men because, in females, the urethra is much shorter and closer to the anus.[16] As a woman's estrogen levels decrease with menopause, her risk of urinary tract infections increases due to the loss of protective vaginal flora.[16] Additionally, vaginal atrophy that can sometimes occur after menopause is associated with recurrent urinary tract infections.[17]
Chronic prostatitis may cause recurrent urinary tract infections in males.[18] Risk of infections increases as males age.[18] While bacteria is commonly present in the urine of older males this does not appear to affect the risk of urinary tract infections.[18]
Urinary catheters
Urinary catheterization increases the risk for urinary tract infections. The risk of bacteriuria (bacteria in the urine) is between three to six percent per day and prophylactic antibiotics are not effective in decreasing symptomatic infections.[16] The risk of an associated infection can be decreased by catheterizing only when necessary, using aseptic technique for insertion, and maintaining unobstructed closed drainage of the catheter.[19][20][21]
Male scuba divers utilizing condom catheters or the female divers utilizing external catching device for their dry suits are also susceptible to urinary tract infections.[22]
Others
A predisposition for bladder infections may run in families. Other risk factors include diabetes,[2] being uncircumcised, and having a large prostate.[3] Complicating factors are rather vague and include predisposing anatomic, functional, or metabolic abnormalities.[23] In children UTIs are associated with vesicoureteral reflux (an abnormal movement of urine from the bladder into ureters or kidneys) and constipation.[7]
Persons with spinal cord injury are at increased risk for urinary tract infection in part because of chronic use of catheter, and in part because of voiding dysfunction.[24] It is the most common cause of infection in this population, as well as the most common cause of hospitalization.[24] Additionally, use of cranberry juice or cranberry supplement appears to be ineffective in prevention and treatment in this population.[25]
Pathogenesis
The bacteria that cause urinary tract infections typically enter the bladder via the urethra. However, infection may also occur via the blood or lymph. It is believed that the bacteria are usually transmitted to the urethra from the bowel, with females at greater risk due to their anatomy. After gaining entry to the bladder, E. Coli are able to attach to the bladder wall and form a biofilm that resists the body's immune response.[5]
Diagnosis
Multiple bacilli (rod-shaped bacteria, here shown as black and bean-shaped) shown between white blood cells in urinary microscopy. These changes are indicative of a urinary tract infection.
 In straightforward cases, a diagnosis may be made and treatment given based on symptoms alone without further laboratory confirmation. In complicated or questionable cases, it may be useful to confirm the diagnosis via urinalysis, looking for the presence of urinary nitrites, white blood cells (leukocytes), or leukocyte esterase. Another test, urine microscopy, looks for the presence of red blood cells, white blood cells, or bacteria. Urine culture is deemed positive if it shows a bacterial colony count of greater than or equal to 103 colony-forming units per mL of a typical urinary tract organism. Antibiotic sensitivity can also be tested with these cultures, making them useful in the selection of antibiotic treatment. However, women with negative cultures may still improve with antibiotic treatment.[2] As symptoms can be vague and without reliable tests for urinary tract infections, diagnosis can be difficult in the elderly.[8]
In straightforward cases, a diagnosis may be made and treatment given based on symptoms alone without further laboratory confirmation. In complicated or questionable cases, it may be useful to confirm the diagnosis via urinalysis, looking for the presence of urinary nitrites, white blood cells (leukocytes), or leukocyte esterase. Another test, urine microscopy, looks for the presence of red blood cells, white blood cells, or bacteria. Urine culture is deemed positive if it shows a bacterial colony count of greater than or equal to 103 colony-forming units per mL of a typical urinary tract organism. Antibiotic sensitivity can also be tested with these cultures, making them useful in the selection of antibiotic treatment. However, women with negative cultures may still improve with antibiotic treatment.[2] As symptoms can be vague and without reliable tests for urinary tract infections, diagnosis can be difficult in the elderly.[8]
Classification
A urinary tract infection may involve only the lower urinary tract, in which case it is known as a bladder infection. Alternatively, it may involve the upper urinary tract, in which case it is known as pyelonephritis. If the urine contains significant bacteria but there are no symptoms, the condition is known as asymptomatic bacteriuria.[3] If a urinary tract infection involves the upper tract, and the person has diabetes mellitus, is pregnant, is male, or immunocompromised, it is considered complicated.[4][5] Otherwise if a woman is healthy and premenopausal it is considered uncomplicated.[4] In children when a urinary tract infection is associated with a fever, it is deemed to be an upper urinary tract infection.[7]
Children
To make the diagnosis of a urinary tract infection in children, a positive urinary culture is required. Contamination poses a frequent challenge depending on the method of collection used, thus a cutoff of 105 CFU/mL is used for a "clean-catch" mid stream sample, 104 CFU/mL is used for catheter-obtained specimens, and 102 CFU/mL is used for suprapubic aspirations (a sample drawn directly from the bladder with a needle). The use of "urine bags" to collect samples is discouraged by the World Health Organization due to the high rate of contamination when cultured, and catheterization is preferred in those not toilet trained. Some, such as the American Academy of Pediatrics recommends renal ultrasound and voiding cystourethrogram (watching a person's urethra and urinary bladder with real time x-rays while they urinate) in all children less than two years old who have had a urinary tract infection. However, because there is a lack of effective treatment if problems are found, others such as the National Institute for Health and Care Excellence only recommends routine imaging in those less than six months old or who have unusual findings.[7]
Differential diagnosis
In women with cervicitis (inflammation of the cervix) or vaginitis (inflammation of the vagina) and in young men with UTI symptoms, a Chlamydia trachomatis or Neisseria gonorrheae infection may be the cause.[3][26] These infections are typically classified as a urethritis rather than a urinary tract infection. Vaginitis may also be due to a yeast infection.[27] Interstitial cystitis (chronic pain in the bladder) may be considered for people who experience multiple episodes of UTI symptoms but urine cultures remain negative and not improved with antibiotics.[28] Prostatitis (inflammation of the prostate) may also be considered in the differential diagnosis.[29]
Hemorrhagic cystitis, characterized by blood in the urine, can occur secondary to a number of causes including: infections, radiation therapy, underlying cancer, medications and toxins.[30] Medications that commonly cause this problem include the chemotherapeutic agent cyclophosphamide with rates of 2 to 40%.[30] Eosinophilic cystitis is a rare condition where eosinophiles are present in the bladder wall.[31] Signs and symptoms are similar to a bladder infection.[31] Its cause is not entirely clear; however, it may be linked to food allergies, infections, and medications among others.[32]Prevention
A number of measures have not been confirmed to affect UTI frequency including: urinating immediately after intercourse, the type of underwear used, personal hygiene methods used after urinating or defecating, or whether a person typically bathes or showers.[2] There is similarly a lack of evidence surrounding the effect of holding one's urine, tampon use, and douching.[16] In those with frequent urinary tract infections who use spermicide or a diaphragm as a method of contraception, they are advised to use alternative methods.[5] In those with benign prostatic hyperplasia urinating in a sitting position appears to improve bladder emptying which might decrease urinary tract infections in this group.[33]
Using urinary catheters as little and as short of time as possible and appropriate care of the catheter when used prevents infections.[19] They should be inserted using sterile technique in hospital however non-sterile technique may be appropriate in those who self catheterize.[21] The urinary catheter set up should also be kept sealed.[21] Evidence does not support a significant decrease in risk when silver-alloy catheters are used
Urinary tract infection
![Urinary tract infection]() Reviewed by Unknown
on
10:31 AM
Rating:
Reviewed by Unknown
on
10:31 AM
Rating:

No comments: